What are the Symptoms of Gestational Diabetes?
Even though the cause is unknown, every year millions of pregnant women are affected by gestational diabetes. It is estimated that between 2% to 10% of pregnancies are diagnosed with gestational diabetes in the United States alone. The condition can cause serious pregnancy complications including stillbirth.
Fortunately, it can be managed very well with a proper diet, exercise and the guidance of a physician. It is also important for women to understand that this is a condition that is not unique to them and they can get support from their healthcare providers, their families, and other support structures.
This article outlines what gestational diabetes is, how it is diagnosed, and ways to self manage and reduce the chances of developing the condition.
What is Gestational Diabetes and its symptoms?
In Gestational Diabetes Mellitus (GDM), like other diabetes types, there is a disruption in the balance (homeostasis) of glucose in the body. It is diagnosed for the first time during pregnancy, commonly in the third trimester, in otherwise healthy women sometimes presenting with typical symptoms of type 2 diabetes (T2DM).
Risk Factors:
Women with the following are at increased risk during pregnancy:
- Over 35 years of age
- Obese or overweight: Having a BMI of 31 or higher
- History of Polycycstic Ovarian Syndrome Ref
- History of Gestational Diabetes
- Family history of GDM, specifically first degree relatives with diabetes
- Being from South East Asia Ref
- Taking certain medications such as corticosteroids and anti-psychotics
These risk factors contribute to the increased risk but do not guarantee that a patient will suffer from GDM at any point during their pregnancy. The more the risk factors a woman has, the higher their risk.
Symptoms:
GDM is often an asymptomatic condition and screening early is the best way to get ahead of it through appropriate treatment and management. However, patients may present with the typical type 2 diabetes (T2DM) symptoms, known as the 4 P’s:
- Polyuria: Urinating more frequently than normal, even having to wake up multiple times at night to urinate. As small amounts of glucose enter the urinary system, it attracts more water to follow it and leave the blood (osmotically active).
- Polydipsia: Excessive thirst, even after drinking a reasonable amount of water. This is caused by the excessive urination that results in dehydration.
- Polyphagia: Excessive eating as a result of increased appetite and hunger. The body is unable to effectively extract the glucose from the blood and signals for higher food intake attempting to bring in more glucose.
- Paresthesia: “Pins-and-needles” sensation usually in the hands and feet. This is not common in early stages.
How is it diagnosed and treated?
Screening & Diagnosis:
Screening should be done at first antenatal visit (6 - 8 weeks) and between 24 and 28 weeks of gestation, especially for women with one or more of the above risk factors.
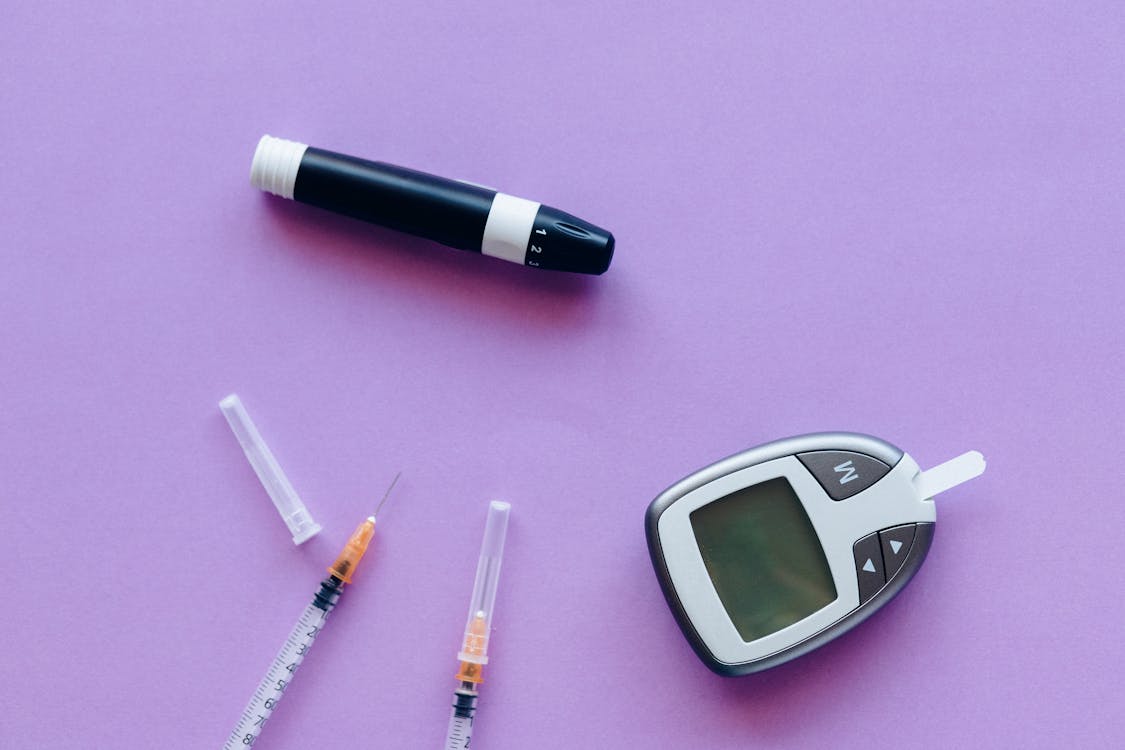
GDM is diagnosed using either blood glucose tests or oral glucose tolerance tests (OGTT). It is clinically diagnosed when the following thresholds are exceeded:
- A Fasting blood glucose of 5.1 mmol/L (92 mg/dL) or greater
- A glucose reading of 10.0 mmol/L (180 mg/dL) or greater after 1 hour using an Oral Glucose Tolerance Test
- A glucose reading of 8.5 mmol/L (153 mg/dL) or greater after 2 hour using an Oral Glucose Tolerance Test
- HbA1c greater than 48 mmol/ml
Treatment & Management:
Management is a multidisciplinary effort requiring attention from an obstetrician, endocrinologist, internist, diabetes educator and neonatologist. Focus is placed on monitoring and improving maternal and fetal well-being.
An array of investigations can be ordered by a diabetic care team to better monitor disease progression. These include, but are not limited to:
- Full Blood Picture
- Blood glucose tests (fasting and/or random)
- Urine tests for ketones, glucose, and protein
- Arterial blood gasses analysis
- Urea, creatinine and electrolytes test
- Glycoslylated Haemoglobin (HbA1c)
- A Lipid Profile test
- Ultrasounds
- Eye examinations
- An ECG
The diabetic care team keeps a close eye on the results of all the investigations as they proceed with treatment, starting with non-pharmacological therapies targeting lifestyle improvements. The point of treatment and management is to control the amount of glucose in a patient’s blood.
A nutritionist will assist with the patient’s dietary therapy through meal planning that restricts fatty foods and simple sugars in the meals to control their caloric intake. Patients are also required to be physically active through regular exercise for at least 30 minutes of moderate intensity aerobic exercise five days a week.
Daily glucose monitoring is highly recommended and patients should take note of their glucose levels when at home using their favorite apps or a simple pen and paper.
What are possible complications?
Complications of GDM can fall into one of three categories:
Maternal Complications:
- Increased risk of C-Section delivery
- Reduced ability to fight infections
- 50% Increased risk of diabetes after delivery
- Insulin related hypoglycaemia
- Increased risk of hypertensive disorders
Fetal Complications:
- Macrosomia (Big baby): Increased glucose access by the fetus accelerates growth and development
- Polyhydramnios (Too much amniotic fluid): As the baby urinates more, the amount of amniotic fluid increases.
- Congenital abnormalities: Imparied body functions or structures present at birth but formed before birth.
- Stillbirth
Infant Complications:
These usually happen during delivery or shortly after.
- Birth Trauma: Due to the large size of the baby, trauma can occur to the child or to the mother’s genital tract
- Hypoglycaemia: Low blood glucose as the child is cut off from mother’s glucose supply and quickly uses up their own glucose.
- Hyperbilirubinemia: Increased bilirubin levels causing yellowing of skin and eyes.
- Hypocalcaemia: Decreased levels of calcium in the blood
- Increased risk of childhood obesity
- Increased risk of respiratory distress syndrome
It is important to communicate often and honestly with your physician to best determine the correct decisions for a healthy pregnancy. In this article we outlined key aspects of gestational diabetes drawing from amazing research and resources all over the internet as referenced where appropriate.